Abstract
Introduction
Systemic therapy with corticosteroids, immunomodulatory agents and/or proteasome inhibitors is the principal treatment modality for plasma cell myeloma. However, some patients with advanced bone disease may start treatment with radiation therapy (RT) to control pain from lytic lesions, fractures, or spinal cord compression. The degree of bone involvement may correlate with cytogenetic lesions, gene expression profile, and prognosis in myeloma (Zhan et al., Blood 2006; Kumar and Rajkumar, Nat Rev Clin Oncol 2018), yet the prognostic relevance of upfront RT use has not been previously studied. We hypothesized that the need for upfront RT may be associated with worse long-term outcomes, as an indicator of late-stage diagnosis or a biologically aggressive disease with bone destruction. Our objective was to examine patterns of use, factors associated with upfront RT, and survival outcomes among myeloma patients treated with upfront RT.
Methods
From the National Cancer Data Base (NCDB), a nationwide registry containing records of >70% of incident cancers in the United States, we selected adult patients with histologically confirmed myeloma diagnosed between 2004 and 2015, who received chemotherapy within 12 months of diagnosis. We excluded patients with solitary plasmacytoma, those treated outside of the reporting facility, or those receiving palliative RT as the only therapy. We defined upfront RT as RT delivered before or within 14 days of the start of chemotherapy. We examined factors associated with upfront RT in a multivariable logistic model. We then examined the association between upfront RT and overall survival (OS) in a proportional hazard model adjusting for age, sex, race, income, insurance status, comorbidity index, year of diagnosis, type of treating hospital, and time from diagnosis to start of therapy.
Results
Of the 88,995 patients with myeloma, 15,223 (18%) received upfront RT, at median 15 days from diagnosis. Median radiation dose was 3000 cGy delivered over median 10 fractions, with the most common targets being spine/skull (59%), hips/pelvis (12%), and other bones (11%). Among patients receiving upfront RT, 73% started it before chemotherapy, while 27% started RT within 14 days of chemotherapy initiation.
Use of upfront RT was significantly less common in academic than community hospitals (16% versus 20%, P<.0001). In the multivariable model, patients receiving upfront RT were significantly younger (odds ratio [OR] for a 10-year age increment: 0.92, 95% CI: 0.91-0.94), more likely to be male (OR: 1.11, 95% CI: 1.07-1.15), white non-Hispanic than black (OR: 1.13, 95% CI: 1.08-1.19), uninsured than privately insured (OR: 1.17, 95% CI: 1.06-1.29), and treated at a community rather than an academic hospital (OR: 1.28, 95% CI: 1.24-1.33). Receipt of upfront RT was also inversely associated with median income in the area of residence, distance to the hospital, and number of comorbidities (P<.0001).
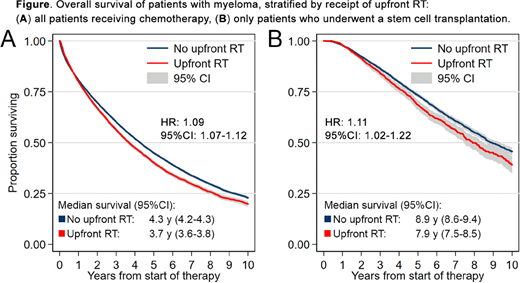
Median OS for the entire cohort was 4.2 years (95% CI, 4.1-4.2), longer for those treated with upfront systemic therapy (4.3 years, 95% CI, 4.2-4.3) than those receiving upfront RT (3.7 years, 95% CI, 3.6-3.8; Fig. A). After adjusting for baseline patient characteristics, treatment with upfront RT was associated with significantly worse OS (hazard ratio [HR]: 1.09, 95% CI: 1.07-1.12). This association was consistent in sensitivity analyses limited to patients who survived >1 year from diagnosis (HR: 1.15, 95% CI: 1.11-1.19), those who underwent autologous stem cell transplantation (HR: 1.11, 95% CI, 1.02-1.22; Fig. B), or accounting for baseline mortality rate using the endpoint of relative survival rather than OS (HR: 1.10, 95% CI: 1.07-1.14).
Conclusions
In this large nationwide cohort, nearly 1 in 5 of newly diagnosed myeloma patients received upfront RT. The association between socio-economic variables like income or insurance status and the use of upfront RT suggests that a delay in diagnosis may lead to severe skeletal complications of myeloma requiring RT. Worse survival with upfront RT may similarly correspond to more advanced disease, but persistent association in sensitivity analyses supports the hypothesis that a presentation with skeletal complications reflects a more aggressive myeloma biology. Further research should aim at disentangling the socio-economic, clinical, and molecular reasons underpinning this association.
Olszewski:Genentech: Research Funding; TG Therapeutics: Research Funding; Spectrum Pharmaceuticals: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal